According to a study recently published in the “Academy of General Dentistry” the so-called temporomandibular disorder and temporomandibular joint dysfunction treatments, consisting of intense pain in the lower jaw along with headaches, may have its origin in poor posture. The report indicates that poor postural habits affect the spine, causing stress on the jaw joint.
Postures such as slouching or sliding back in the seat cause the lower jaw to move forward and the lower and upper teeth to not fit together correctly. The skull is positioned backward and all the weight falls on the first vertebrae of the spine, an unnatural position.
This type of posture causes tension in the muscles, bones, and joints that, if not treated by a specialist in time, can lead to inflammation of the muscles and joints when we carry out the basic movement of the jaw, which is to open and close the mouth, a movement without which we could not eat.
Therefore, the main reading that we must make from this study is that we must take great care of the postures we adopt since it is of vital importance for our health in general, and our oral health in particular because back pain is related to problems dental.
Adopting a good posture at work, or in the place where we spend most of the day, and also at home when we rest, is something that we must mechanize to always be sitting correctly. If we have bad postures we must correct them so that the problem does not worsen and we avoid a possible misalignment of the jaw.
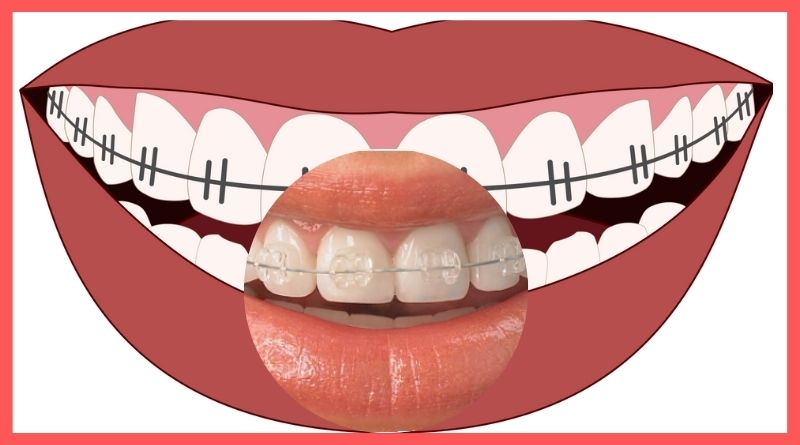
In these cases, dental experts recommend the use of oral appliances so that the teeth can be aligned in their original position, and in this way, the jaw pain caused by poor posture will be considerably reduced, in addition to preventing possible damage to the teeth that can be easily avoided just by paying attention to your posture.
What are TMJ disorders?
They are conditions that generate pain and dysfunction in the jaw joint and also in the muscles that facilitate jaw movement. They occur when the jaw contracts and the teeth are ground, which puts greater pressure on the jaw muscles, causing inflammation.
It is the joint originating from the upper part of the jaw and the temporal bone of the skull. It acts like a sliding hinge and can manifest problems caused by the movements it makes to fulfill its function.
All people have two TMJs, one on each side of the face, which connect the jaw and skull and allow us to freely move and open our mouths normally.
Generally, a person should be able to open the oral cavity with a distance between 40 and 50 centimeters. To check that the TMJ does not suffer any complications, a simple test can be applied by inserting three fingers vertically between the central and lower incisors.
How are TMJ disorders classified?
Dentists have divided temporomandibular dysfunction into three categories:
*Myofascial pain
It has to do with discomfort or pain in the muscles that work for the correct functioning of the jaw.
*internal joint disorder
This is a displaced disc that involves a dislocation of the jaw or injury to the condyle. It is an element that articulates with the cranial base; For its part, the disc has the function of cushioning the movements of the joint parts.
*Arthritis
It encompasses a group of degenerative or inflammatory disorders of the joints that cause damage to the TMJ. Specifically, patients with rheumatoid arthritis are the most likely to suffer from temporomandibular dysfunction compared to healthy patients.
Diagnosis of temporomandibular joint (TMJ) disorder
The diagnosis of TMJ is made, first, through an objective examination by the dentist, followed by specialized tests such as x-rays, CT scans, or MRIs to confirm the problem.
During the examination, the specialist will check for joint clicking or muscle pain by placing his fingers on the patient’s face while he opens and closes his mouth. This evaluation will also check for an abnormal opening or dislocation of the jaw.
Temporomandibular joint dysfunction symptoms
Symptoms that may indicate a problem in the temporomandibular area are mainly pain when chewing, headaches, abnormal noises produced by the joints in the affected area and even blocking of the jaw.
In more advanced cases, the pain can also extend to the neck and arm area, causing contractures, dizziness, a sensation of clogged ears, and restless sleep.
Very often, when you suffer from temporomandibular disorders, you have the feeling that the perceived pain comes from the vicinity of the joint and not from the joint itself. However, symptoms such as headaches caused by this condition do not respond to conventional treatment.
In summary, the most common temporomandibular joint dysfunction symptoms are:
*Pain or discomfort when chewing.
*Headache.
*Ear pain or feeling of clogged ears.
*Abnormal noise when opening and closing the mouth.
*Difficulty opening and closing the mouth.
*Shoulder and neck stiffness.
*Dizziness
*Sleep disorders.
What causes temporomandibular dysfunction
Temporomandibular dysfunction is an Evolutionary Disease of the Human Masticatory System that our current society perpetuates, in part, due to eating habits.
What does this mean? In addition to being caused by the decrease in our jaw during evolution, our diet also bears part of the responsibility.
Everything or almost everything we eat since we were children is cooked so that we do not have to chew or so that chewing is softer. We no longer tear up pieces of meat like our ancestors did, but we eat meatballs and hamburgers or we cook the meat so that it is tender and soft, we eat cut and peeled fruit, bags of lettuce with tender sprouts, and vegetable creams… Anyway, the list is endless.
This affects our bone and jaw muscle development from a young age.
Different types of arthritis, such as rheumatoid arthritis or osteoarthritis, can also be causes of temporomandibular syndrome.
We cannot guarantee the prevention of jaw dysfunction, but we can give you some basic advice that can help from childhood:
1. To the extent possible, extending breastfeeding can be useful for bone and muscle development, since expressing milk requires more effort than through the bottle’s nipple.
2. Try to get children used to chewing harder or more fibrous foods, reducing the consumption of creams and purees or sliced bread, for example. Promote the use of the incisors when chewing crusty breads and meat steaks, fruit with uncut skin… In short, trying to make chewing an effort for the little ones can reduce the chances of suffering from temporomandibular joint disorder in adults.
3. Insist that they practice conscious chewing, that is, try to use both sides of the mouth when eating to avoid asymmetries and jaw dysfunction.
4. Another piece of advice is to ensure that children (also applicable to adults) do not sleep on their side, with their hand under their face or pillow, or face down, since with these positions we are exerting lateral pressure on the jaw and favoring The appearance of a crossbite, which also requires orthodontics to reverse, may also be related to temporomandibular joint disorder.
Summary of TMJ Causes:
*Dental problems (poor dental alignment, bite alterations)*Stress: By contracting the jaw generally, during night rest, or due to stressful circumstances, grinding the teeth adds more pressure to the jaw muscles.
Temporomandibular joint dysfunction treatments
In certain cases, the symptoms disappear without the need for treatment, but if they persist the dentist may recommend:
*Pain relievers and anti-inflammatories
If the temporomandibular pain does not subside with over-the-counter pain relievers, the specialist will prescribe stronger medications for a limited period, for example, prescription ibuprofen.
*Tricyclic antidepressants
Medications such as amitriptyline are used to treat depression, but in adequate doses, they are recommended to relieve pain, control bruxism, and eradicate insomnia.
*Muscle relaxants
They are usually used for a few days, or even weeks, to relieve the pain of TMJ disorders due to muscle spasms.
*Discharge splint:
If the determining cause is bruxism, the specialist will recommend that the patient use a relief splint that facilitates relaxation of the jaw.
*Physiotherapy
This treatment is added to exercises to stretch and strengthen the jaw muscles, including ultrasound, ice, and moist heat.
*Arthrocentesis surgery
If the pain does not subside, the maxillofacial surgeon or dentist will likely recommend this surgery, which consists of a minimally invasive procedure that inserts small needles into the joint to irrigate fluid through it, eliminating waste.
*Botulinum toxin injections
Corticosteroid injections are very useful in these cases. In some patients, botulinum toxin type A injection is applied around the jaw muscles that work in chewing, only if TMJ disorders are still evident.
*Open joint surgery
If the pain is not resolved with conventional treatments and it is detected that its origin is structural in the joint, the maxillofacial surgeon or dentist may suggest this surgery, also called arthrotomy, which consists of repairing or replacing the joint. It is important to remember that this procedure involves more risks than other treatments and you must be fully aware of the recovery processes, previously detailed by the maxillofacial surgeon or dentist.
Non-surgical temporomandibular joint dysfunction treatments
There are different possibilities. When the disorder is caused by bruxism or the habit of clenching the teeth, it is usual to recommend the use of a relief splint. Avoiding chewing hard foods, applying cold or heat to the area, or taking medications to relieve pain and reduce inflammation are also conservative treatments.
When the origin of TMJ disorders is malocclusions, the recommendation will be to start some orthodontic treatment. And, in the absence of teeth, their replacement will be necessary, with bridges or, if possible, implants.
Finally, it is possible to follow a myofunctional therapy treatment. It is suitable for improving joint mobility, working on the chewing pattern, or relaxing the muscles. All of this contributes to relieving discomfort in the TMJ, correcting harmful habits, and improving the quality of life of patients with severe alterations.
Surgical temporomandibular joint dysfunction treatments
Sometimes, it is necessary to go to surgery to control symptoms or recover joint functionality. There are also different alternatives.
One of them is TMJ arthrocentesis, a minimally invasive treatment that involves draining fluid from the joint while pumping fluid into it. In this way, it is possible to return the condylar disc to its place when it has moved.
Arthroscopy is another surgical procedure, although more aggressive. It consists of introducing a small instrument into the joint that allows the specialist to see it, remove tissues, or place the disc if necessary.
Only in very specific cases will it be necessary to perform more complex treatments, such as open surgery or the placement of prostheses in the joint.
Temporomandibular joint dysfunction treatments combined
In cases of mild bruxism, the problem can disappear on its own, without even causing a disorder in the TMJ. Many children end up overcoming bruxism without needing to see a specialist. In the case of adults, sometimes the grinding is so mild that it does not cause symptoms and does not require specific treatment.
In cases where bruxism is more serious, it is necessary to see a specialist:
The idea is not to let time pass to prevent the symptoms from worsening. In this way, it will be easier to address the problem and we will achieve a better recovery by minimizing the damage that may occur, such as dental wear or the loss of a piece.
The most appropriate bruxism treatment requires a multidisciplinary approach, which may require the following specialists:
Physiotherapist specialized in TMJ
The physiotherapist specializing in TMJ physiotherapy will work with the patient to reduce the symptoms associated with TMJ disorder and dysfunction, such as pain, jaw blockage, the existence of contractures derived from the tension exerted on the jaw muscles, etc… In this way, you will achieve symptomatic relief and greater comfort for the patient.
Dentist for temporomandibular joint dysfunction treatments
When there is a problem of malocclusion due to incorrect alignment of the teeth, orthodontics is the most appropriate solution. In cases where there is no misalignment of the teeth, the dentist may recommend a relief splint that the patient should wear at night. With the splint, the superficial wear on the teeth will be stopped, but it will be necessary to analyze the underlying pathology.
Specialist in sleep medicine
When bruxism stems from a significant problem with sleep, the diagnosis should begin with a complete sleep study. To do this, the specialist will analyze the episodes of teeth grinding that the patient suffers while sleeping, to determine if there are episodes of apnea or other disorders.
Psychologist for temporomandibular joint dysfunction treatments
When the bruxism problem has an emotional component, a specialist who treats the underlying problem of stress, anxiety, etc. will also be required. In these cases, treatment will be aimed at controlling stress and anxiety.
What consequences does temporomandibular dysfunction have?
A person who suffers from temporomandibular joint disorders will have very persistent disorders in the jaw area, which will prevent the patient from developing a normal life:
*Swallowing problems
Limitations when eating are one of the main problems since you will have difficulties opening your mouth naturally, complicating chewing food.
*Failures in oral hygiene
Your oral cleaning routine will be seriously affected since you will probably not be able to see the back teeth, which makes it difficult to care for your molars and floss.
*Speech problems
Patients with TMJ disorders also suffer from different disorders when moving their jaw to speak, since muscle rigidity can make it difficult to pronounce some telephone messages, even causing pain.
Tips for temporomandibular joint (TMJ)
Despite advances in the treatment of this disorder, it is important to follow a series of basic tips:
*Avoid hard foods that require a long period of chewing, especially those that require opening the mouth widely or making chewing efforts.
*Avoid improper and excessive use of the jaw (for example, avoid eating gum, or pipes…)
*If possible, avoid grinding or clenching your teeth. If you clench or grind your jaw during sleep, go to the dentist to have a relief splint made.
*Avoid stress as much as possible or seek some type of help to reduce it (relaxation, psychological therapy, pharmacological therapy, etc.)
*Frequently massage the joint or painful areas using direct pressure with your fingers or making circles. It is highly advisable to seek the advice and treatment of a physiotherapist with knowledge of manipulation of the temporomandibular joint.
*Apply heat to the painful areas, with a hot cloth or an electric blanket, for about fifteen minutes, once or twice a day, especially in cold weather.
*Consult with the dentist to improve the alignment of the teeth as much as possible, replacing lost teeth with prostheses and fixing damaged ones. This will ensure that chewing is done correctly and that jaw movements are carried out following the correct “dental guides”, so as not to cause damage and pain in the joint.
*During the periods in which the pain becomes more intense, it is advisable to eat the softest foods possible (pores), limit jaw movements as much as possible, and go to the doctor to prescribe the appropriate treatment (generally it consists of a combination of analgesics, anti-inflammatories, and muscle relaxants)
When should you go to the dentist for temporomandibular joint disorder
Seek medical attention if you have persistent tenderness or pain in your jaw. The dentist will analyze the possible causes and treatments for the problem.
As we mentioned at the beginning, treatments are usually quite simple, since, in most cases, they do not require surgery. Intraoral appliances or techniques may be used to correct jaw posture.
Risk factors of temporomandibular joint dysfunction treatments
Some factors can increase the risk of suffering from this disorder:
*Different types of arthritis.
*Long-term teeth grinding or clenching ( bruxism ).
*Connective tissue diseases that cause problems that can affect the temporomandibular joint.
Maintaining our joints’ health is very important since they allow us to move with as much freedom as possible. These injuries can be avoided with prevention and regular visits to your dentist to detect risk factors such as bruxism as soon as possible.
Conclusion of temporomandibular joint disorder
The temporomandibular joint disorder primarily affects the temporalis muscle and jaw movements, causing functional limitations in terms of the range of movement.
For you to understand what temporomandibular joint disorder consists of, it is necessary to know the bone morphology of the face. The temporomandibular joints connect the temporal bones of the skull and the lower jaw bone. We have two temporomandibular joints (one on each side) in front of our ears.
These joints are supported by ligaments, tendons, and muscles (known as temporal muscles) that allow us to perform jaw movements, such as opening and closing the mouth. Let’s say that the temporomandibular joint acts as a hinge to open and close the mouth.
Well, with this understood, mandibular dysfunction occurs when the space in the oral cavity is not enough for the jaw to perform these movements normally. The temporalis muscle can become trapped in the zygomatic foramen, and given its proximity, the mandible hits the upper jaw. In certain patients, this movement produces a clicking sound.
The impact produces nervous sensitization, making it difficult or generating pain in natural activities such as speaking, eating, or swallowing food.
This dysfunctional movement causes inflammation and discomfort, which triggers many other symptoms, such as headaches, migraines, dizziness, and vertigo, among other symptoms.
Diseases such as Meniere’s Syndrome, Trigeminal Neuralgia, Peripheral Facial Paralysis, or Burning Mouth Syndrome, among others, may have their origin in the masticatory system, but until now, there is a specialization in Temporomandibular Joint Disorder has not been discovered.
In fact, on many occasions, we find CAT patients who have not been diagnosed and are referred to other specialists after years of searching for a solution to their problem and having visited all types of doctors and healthcare providers, from ENT doctors and neurologists to physiotherapists and psychologists.
Not finding the cause of their discomfort or even having found specialists who doubted whether their symptoms were real or the product of a psychological disorder, they feel a certain despair.
Read more: Bacterial plaque on teeth, causes, looks likes and prevents
Please subscribe to my channel and follow